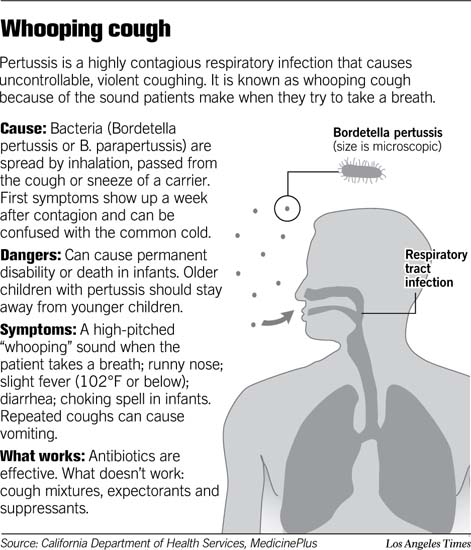
Whooping cough (pertussis) is an infection of the respiratory system caused by the bacterium Bordetella pertussis (or B. pertussis). It’s characterized by severe coughing spells, which can sometimes end in a “whooping” sound when the person breathes in.
It mainly affects infants younger than 6 months old before they’re adequately protected by immunizations, and kids 11 to 18 years old whose immunity has started to fade.
Before a vaccine was available, pertussis killed 5,000 to 10,000 people in the United States each year. Now, the pertussis vaccine has reduced the annual number of deaths to less than 30. But in recent years, the number of cases has started to rise. By 2004, the number of whooping cough cases spiked past 25,000, the highest level it’s been since the 1950s.
Signs and Symptoms
The first symptoms of whooping cough are similar to those of a common cold:
- runny nose
- sneezing
- mild cough
- low-grade fever
After about 1 to 2 weeks, the dry, irritating cough evolves into coughing spells. During a coughing spell, which can last for more than a minute, the child may turn red or purple. At the end of a spell, the child may make a characteristic whooping sound when breathing in or may vomit. Between spells, the child usually feels well.
Although many infants and younger children who become infected with B. pertussis will develop the characteristic coughing episodes and accompanying whoop, not all will. And sometimes infants don’t cough or whoop as older kids do. Infants may look as if they’re gasping for air with a reddened face and may actually stop breathing (called apnea) for a few seconds during particularly bad spells.
Adults and teens with whooping cough may have milder or atypical symptoms, such as a prolonged cough (rather than coughing spells) or coughing without the whoop.
Contagiousness
Pertussis is highly contagious. The bacteria spread from person to person through tiny drops of fluid from an infected person’s nose or mouth. These may become airborne when the person sneezes, coughs, or laughs. Others then can become infected by inhaling the drops or getting the drops on their hands and then touching their mouths or noses.
Infected people are most contagious during the earliest stages of the illness for up to about 2 weeks after the cough begins. Antibiotics shorten the period of contagiousness to 5 days following the start of antibiotic treatment.
Prevention
Whooping cough can be prevented with the pertussis vaccine, which is part of the DTaP (diphtheria, tetanus, acellular pertussis) immunization. DTaP immunizations are routinely given in five doses before a child’s sixth birthday. To give additional protection in case immunity fades, the American Academy of Pediatrics (AAP) now recommends that kids ages 11-18 get a booster shot of the new combination vaccine (called Tdap), ideally when they’re 11 or 12 years old, instead of the Td booster routinely given at this age.
The Tdap vaccine is similar to DTaP but with lower concentrations of diphtheria and tetanus toxoid. It also can be given to adults who did not receive it as preteens or teens. This is especially important for those who are in close contact with infants, because babies can develop severe and potentially life-threatening complications from whooping cough. An adult’s immunity to whooping cough lessens over time, so getting vaccinated andprotecting yourself against the infection also helps protect your infant or child from getting it.
As is the case with all immunization schedules, there are important exceptions and special circumstances. Your doctor will have the most current information.
Experts believe that up to 80% of nonimmunized family members will develop whooping cough if they live in the same house as someone who has the infection. For this reason, anyone who comes into close contact with someone who has pertussis should receive antibiotics to prevent spread of the disease. Young kids who have not received all five doses of the vaccine may require a booster dose if exposed to an infected family member.
Incubation
The incubation period (the time between infection and the onset of symptoms) for whooping cough is usually 7 to 10 days, but can be as long as 21 days.
Duration
Pertussis usually causes prolonged symptoms — 1 to 2 weeks of common cold symptoms, followed by 2 to 4 weeks (sometimes more) of severe coughing.
The last stage consists of another few weeks of recovery with gradual clearing of symptoms. In some children, the recovery period can last for months.
Professional Treatment
Call the doctor if you suspect that your child has whooping cough. To make a diagnosis, the doctor will take a medical history, do a thorough physical exam, and take nose and throat mucus samples that will be examined and cultured for B. pertussisbacteria. Blood tests and a chest X-ray also might be done.
A confirmed case of whooping cough will be treated with antibiotics, usually for 2 weeks. Many experts believe that the medication is most effective in shortening the duration of the infection when given in the first stage of the illness, beforecoughing spells begin. But even if antibiotics are started later, they’re still important because they can stop the spread of the pertussis infection to others. Ask your doctor whether preventive antibiotics or vaccine boosters for other family members are needed.
Some kids with whooping cough need to be treated in a hospital. Infants and younger children are more likely to be hospitalized because they’re at greater risk for complications such aspneumonia, which occurs in about 1 in 5 children under the age of 1 year who have pertussis. Up to 75% of infants younger than 6 months old with whooping cough will receive hospital treatment. In infants younger than 6 months of age, whooping cough can even be life threatening.
Other potential complications include difficulty breathing, periods of apnea, needing oxygen particularly during a coughing spell, and dehydration due to poor oral intake.
While in the hospital, a child may need suctioning of thick respiratory secretions. Breathing will be monitored and oxygen given, if needed. Intravenous (IV) fluids might be required if a child shows signs of dehydration or has difficulty eating. Precautions will be taken to prevent the infection from spreading to other patients, hospital staff, and visitors.
Home Treatment
If your child is being treated for pertussis at home, follow the schedule for giving antibiotics exactly as your doctor prescribed. Giving cough medicine probably will not help, as even the strongest usually can’t relieve the coughing spells of whooping cough. The cough is actually the body’s way of trying to clear respiratory secretions. (Due to potential side effects, cough medicines are never recommended for children under age 6.)
During recovery, let your child rest in bed and use a cool-mist vaporizer to help loosen respiratory secretions and soothe irritated lungs and breathing passages. (Be sure to follow directions for keeping it clean and mold-free.) In addition, keep your home free of irritants that can trigger coughing spells, such as aerosol sprays; tobacco smoke; and smoke from cooking, fireplaces, and wood-burning stoves.
Kids with whooping cough may vomit or not eat or drink much because of the coughing. So offer smaller, more frequent meals and encourage your child to drink lots of fluids. Watch for signs of dehydration, too, including thirst, irritability, restlessness, lethargy, sunken eyes, a dry mouth and tongue, dry skin, crying without tears, and fewer trips to the bathroom to pee (or in infants, fewer wet diapers).
When to Call the Doctor
Call the doctor if you suspect that your child has whooping cough or has been exposed to someone with whooping cough, even if your child has already received all scheduled pertussis immunizations.
Your child should be examined by a doctor if he or she has prolonged coughing spells, especially if these spells:
- make your child’s skin or lips turn red, purple, or blue
- are followed by vomiting
- are accompanied by a whooping sound when your child breathes in after coughing
- is having difficulty breathing or seems to have brief periods of not breathing (apnea)
- is lethargic
If your child has been diagnosed with whooping cough and is being treated at home, seek immediate medical care if he or she has difficulty breathing or shows signs of dehydration.
Source: KidsHealth